Understanding and Managing Graves’ Disease
Dr. Klyde provides comprehensive evaluation and long-term management for patients with Graves’ disease, a thyroid condition that causes overproduction of thyroid hormones. He works with patients throughout New York City and the Tri-State area to develop individualized treatment plans focused on symptom control, long-term health, and quality of life.
Graves Disease and Hyperthyroidism
General
Graves’ disease is the most common cause of hyperthyroidism, a condition in which the thyroid gland produces excessive amounts of thyroid hormone. Other causes of hyperthyroidism include autonomously functioning thyroid nodules—often referred to as “hot” nodules within a multinodular goiter—and thyroid inflammation (thyroiditis), which can cause a temporary release of stored thyroid hormones into the bloodstream. While thyroiditis typically resolves on its own over time, Graves’ disease and hyperfunctioning nodules generally worsen without appropriate treatment.
Graves’ disease is an autoimmune disorder. In this condition, the immune system produces antibodies that stimulate the thyroid gland to overproduce the hormones thyroxine (T4) and triiodothyronine (T3). These hormones regulate metabolism and influence many body systems, including the heart, muscles, bones, and nervous system. When hormone levels become excessive, patients may experience symptoms such as palpitations, heat intolerance, weight loss, tremor, anxiety, fatigue, and changes in sleep or concentration.
Although Graves’ disease is less common than Hashimoto’s thyroiditis, the most frequent autoimmune thyroid disorder, it shares a similar autoimmune origin. In Hashimoto’s disease, different antibodies interfere with thyroid function and typically lead to hypothyroidism, or underactive thyroid function. Both conditions can occur within the same family, and in some cases, an individual may experience features of both disorders at different points in life.
Graves’ disease can also affect tissues outside the thyroid. Some patients develop eye symptoms, known as Graves’ ophthalmopathy or thyroid eye disease, which may cause eye irritation, dryness, swelling, or changes in appearance. Less commonly, skin changes may occur. Because symptoms and severity can vary widely, careful evaluation and individualized management by an endocrinologist are essential.
With proper diagnosis and treatment, Graves’ disease is highly manageable. An endocrinologist can help determine the underlying cause of hyperthyroidism, explain treatment options, and guide long-term care to restore hormonal balance and protect overall health.
Symptoms
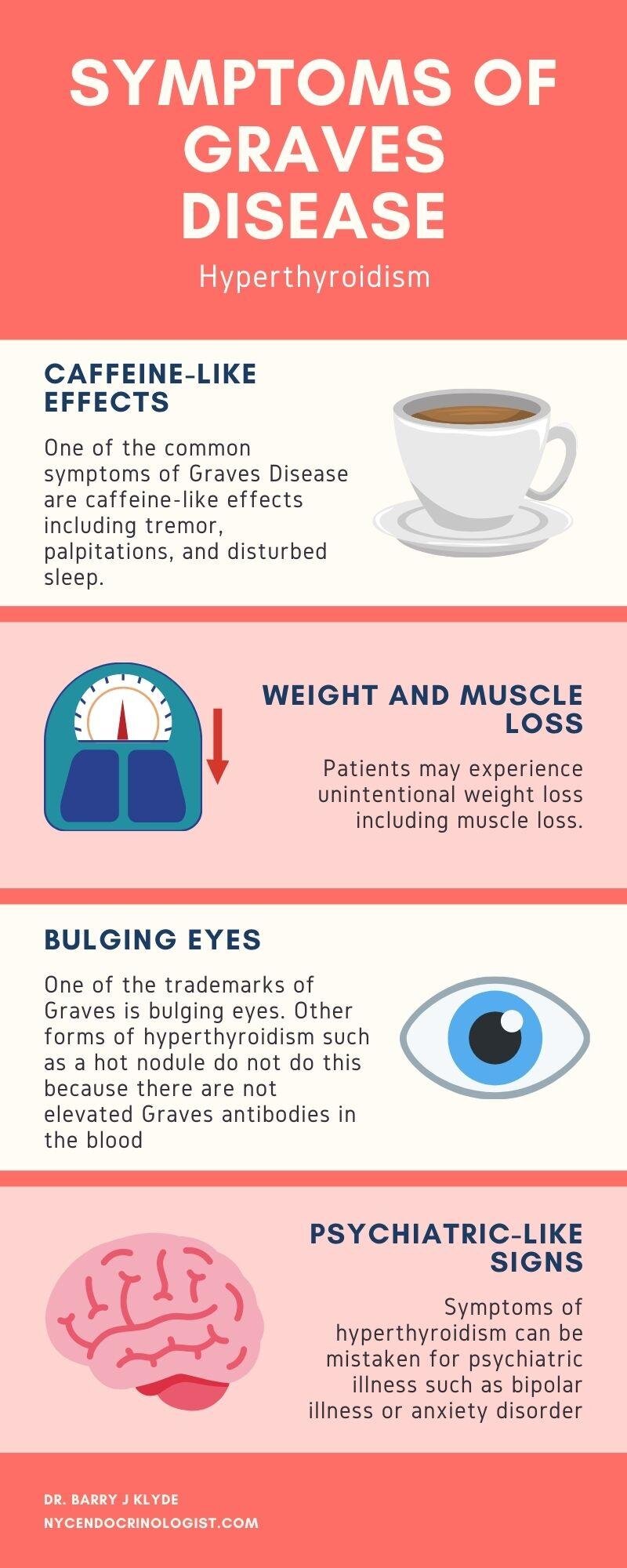
Graves’ disease most commonly presents with symptoms of hyperthyroidism, which reflect the body’s response to excess thyroid hormone. Many patients describe these effects as similar to consuming too much caffeine. Common early symptoms include tremor, heart palpitations, restlessness, and difficulty sleeping. As thyroid hormone levels remain elevated, patients may experience unintentional weight loss despite a normal or increased appetite, loss of muscle mass, heat intolerance with excessive sweating, and increased fatigue.
Changes in mood and cognition are also common. Patients may notice heightened anxiety, irritability, emotional lability, or difficulty concentrating. Because these symptoms can overlap with psychiatric conditions such as anxiety disorders or bipolar disorder, hyperthyroidism is sometimes misdiagnosed. Similarly, hypothyroidism often characterized by fatigue, lethargy, and weight gain, can be mistaken for depression, highlighting the importance of appropriate medical evaluation.
Additional physical signs of hyperthyroidism may include warm or oily skin, fine or thinning scalp hair with increased breakage, separation or brittleness of the fingernails, and more frequent bowel movements that are typically formed rather than loose. Some patients also notice changes in menstrual cycles or decreased exercise tolerance due to cardiovascular effects.
Graves’ disease has features that distinguish it from other causes of hyperthyroidism. In some individuals, antibodies associated with Graves’ disease affect tissues outside the thyroid gland, particularly the muscles and connective tissue around the eyes. This can lead to thyroid eye disease, also known as Graves’ ophthalmopathy, which may cause eye irritation, dryness, redness, swelling, or a protruding appearance of the eyes (exophthalmos). These eye findings are specific to Graves’ disease and do not occur in other forms of hyperthyroidism, such as autonomously functioning (“hot”) thyroid nodules, where Graves’ antibodies are not present.
The severity and combination of symptoms can vary widely from person to person. Some individuals experience subtle or slowly progressive changes, while others develop more pronounced symptoms over a shorter period of time. An endocrinologist can help distinguish Graves’ disease from other conditions, confirm the diagnosis, and guide appropriate treatment based on each patient’s presentation and needs.
Diagnosis
Diagnosis of hyperthyroidism is made by hearing about the typical symptoms, and finding rapid heartbeat, tremor, sweats, enlarged thyroid or goiter, and skin, nail and hair changes on exam. Graves disease would cause a diffusely enlarged goiter, while a hot nodule would be suggested by finding an irregularly enlarged nodular goiter on exam. Observation of bulging eyes, or exophthalmos, would indicate that the hyperthyroidism is likely from Graves disease rather than a hot nodule. Laboratory tests would show elevation of the thyroid hormones T4 and T3, with suppression of TSH. If the cause is Graves disease then the antibodies TSI and TRAB may be elevated, but they may be seemingly normal even if Graves disease is the cause of hyperthyroidism.
Treatment
The choice of treatment depends on different factors. The overactive gland can be surgically removed, it can be destroyed with radioactive iodine, or suppressed with anti-thyroid medication. Anti-thyroid drugs used for a year may produce a cure in up to half of patients with Graves disease, but may have the side effects of rash, gastrointestinal symptoms, liver disease, or rarely suppress production of white blood cells in the bone marrow and lead to life-threatening infection. Anti-thyroid drugs might only produce temporary benefit in hot nodules so are not appropriate in that circumstance. Radioactive iodine will eliminate hyperthyroidism in both Graves disease and hot nodules, but with a high chance of causing the opposite problem, hypothyroidism, with need for lifelong thyroid medication such as Synthroid. Surgery is used in special circumstances, such as in pregnancy where radioactive iodine cannot be given because of an effect on the fetus, or when it is important to quickly correct the thyroid hormone excess, as in serious heart disease, or if there is severe exophthalmos. It is important to use experience and good clinical judgement to balance benefit and risk to decide on the best therapy.